What to Expect in a Physiotherapy Session


Physiotherapy is one of the most trusted healthcare options for pain management, recovering from injury, and improving mobility. Whether you’re an athlete, an office worker, or someone dealing with long-term pain, physiotherapy provides tailored treatment to help you move better and live with less discomfort.
For many people, though, the first physiotherapy appointment can feel daunting. Not knowing what will happen during your initial session can create unnecessary anxiety.
This guide walks you step-by-step through the initial assessment, physiotherapy assessment process, treatment techniques, and outcomes, helping you understand what to expect from your first appointment so you can arrive prepared and confident.
Who Can Benefit from Physiotherapy?
- Athletes recovering from sports injuries.
- Older adults managing chronic pain or reduced mobility.
- Office workers dealing with poor posture or ergonomic strain.
- Parents supporting children with musculoskeletal concerns.
- Anyone experiencing pain or restricted movement.
Physiotherapy is a safe, professional, and evidence-based way to support your body’s recovery and long-term health.
What Happens at Your First Physiotherapy Appointment?
Initial Consultation and Patient History


Your first physiotherapy appointment begins with an objective assessment and conversation. The physiotherapist will ask about:
- Your current symptoms.
- Previous injuries or medical history.
- Lifestyle factors such as work, sport, and activity levels.
- What you’d like to achieve from treatment.
This step is crucial to understanding your body and setting realistic goals.
Physical Examination and Assessment
After gathering your history, the physiotherapist will complete a physical examination as part of the physical assessment. This might include:
- Range of motion testing.
- Posture and movement analysis.
- Strength and flexibility checks.
- Neurological or functional assessments (if relevant).
This helps pinpoint the root cause of your pain or restriction, not just the symptoms.
Goal Setting: Short and Long Term
Together, you and your physiotherapist will set achievable goals, such as incorporating specific exercises into your program.
- Short-term: reducing pain or swelling.
- Long-term: restoring function, returning to sport, or improving mobility.
How Long Is a Physiotherapy Session?
Initial appointments often run between 45–60 minutes, as they involve assessment plus treatment.
Follow-up appointments usually last 30 minutes, focusing more on treatment and progression.
Follow-Up Sessions: What to Expect
Reviewing Your Progress
Every follow-up physiotherapy session begins with a review of how you’ve been feeling since your last visit. Your physiotherapist will ask about any changes in pain, improvements in mobility, or difficulties completing home exercises. This is your chance to share what’s working well and highlight any challenges you’ve faced. By tracking progress, your physiotherapist can identify patterns, celebrate improvements, and adjust your treatment plan if necessary. These regular reviews ensure that each session is tailored to your evolving needs and that you remain on the right path toward achieving your recovery goals.
Progressing the Treatment Plan
Physiotherapy is not a one-size-fits-all process—it evolves as your body heals and adapts. During follow-up sessions, your physiotherapist will assess whether you are ready for more advanced techniques, increased exercise intensity, or new movement strategies. For example, once pain is under control, your plan may shift towards rebuilding strength, balance, and endurance. This progression ensures you are constantly moving closer to full recovery while avoiding setbacks.
Home Exercises and Self-Management


One of the most important parts of physiotherapy happens outside the clinic. Your physiotherapist will provide you with simple, tailored exercises to perform at home, often focusing on stretching, strengthening, or posture correction. In addition, you may receive guidance on ergonomics, lifestyle changes, or activity modifications to support your recovery. This active participation speeds up healing and helps you maintain results long-term. By committing to your home program, you become a key partner in your recovery journey, ensuring that the benefits of each session are reinforced daily. Consistency here can make the difference between short-term relief and lasting results.
What a Typical Follow-Up Looks Like
Follow-up sessions are generally more treatment-focused and efficient than your initial appointment. They usually begin with a brief check-in on your symptoms, followed by hands-on techniques such as manual therapy or guided exercise. Your physiotherapist may then introduce new strategies or refine your current program, depending on how you’re progressing. Before you leave, you’ll receive guidance on home exercises or self-care practices to continue between sessions, as well as details on what to expect at your next appointment . Finally, your physiotherapist will outline the next stage of your recovery plan, so you know what to expect moving forward. This structured approach ensures continuity, clarity, and confidence in your treatment journey.
Common Physiotherapy Treatment Techniques
Manual Therapy
Manual therapy is a cornerstone of physiotherapy and involves the physiotherapist using their hands to directly treat your muscles, joints, and soft tissues. This can include techniques such as joint mobilisation, soft tissue massage, and gentle manipulations designed to reduce stiffness, ease tension, and improve the way your body moves. Unlike a general massage, manual therapy is highly targeted and tailored to your individual needs based on your assessment.
The main goal of manual therapy is to restore normal movement patterns, reduce pain, and improve function. For example, if you have a stiff shoulder after an injury, your physiotherapist may use specific joint mobilisations to loosen the joint capsule while also working on surrounding muscles to relieve tightness. This combination can help you move more freely and comfortably.
Manual therapy is particularly effective for conditions such as neck and back pain, joint restrictions, sports injuries, and postural issues. It often works best when paired with exercise therapy, as improving joint mobility alone won’t prevent symptoms from returning without strengthening the body. Patients usually find manual therapy relaxing, and many report immediate relief from stiffness and discomfort after treatment.
Exercise Therapy
Exercise therapy is one of the most important aspects of physiotherapy because it equips patients with the tools to manage their own recovery. Instead of only treating the symptoms, exercise therapy focuses on correcting imbalances, improving strength, increasing flexibility, and restoring proper movement patterns. Physiotherapists prescribe exercises specifically tailored to your needs, meaning the program you receive is unique to your body, condition, and goals.
For example, someone recovering from a knee injury may be prescribed strengthening exercises for the quadriceps and glutes, while an office worker with poor posture may focus on core stability and spinal mobility. These exercises can range from gentle stretches to more advanced strengthening or balance drills, depending on where you are in your recovery journey.
The benefits of exercise therapy go beyond the clinic and support the recovery process . By performing your exercises at home, you help reinforce the progress made in your sessions and reduce the likelihood of recurring injuries. Exercise therapy is also essential for long-term prevention, particularly for athletes who want to stay strong and avoid repeated setbacks. Consistency is key, and your physiotherapist will adapt your program as you progress to ensure you keep moving forward safely.
Electrotherapy & Ultrasound


Electrotherapy and ultrasound are specialised techniques that some healthcare professionals, including physiotherapists, use to complement manual and exercise-based treatments. Electrotherapy involves using small electrical currents to stimulate nerves and muscles. Common methods include TENS (Transcutaneous Electrical Nerve Stimulation) for pain relief and NMES (Neuromuscular Electrical Stimulation) to help retrain weakened muscles. These treatments can be especially useful for people recovering from injury or surgery where muscle activation is limited, and may be complemented by additional scans to assess progress .
Ultrasound therapy, on the other hand, uses sound waves to penetrate tissues beneath the skin. This process creates a gentle warming effect that can improve blood circulation, reduce inflammation, and promote tissue healing. It is often used for soft tissue injuries, tendon problems, or scar tissue management.
These modalities are not used in every physiotherapy clinic or for every patient. Instead, they are applied when evidence suggests they may support your recovery goals. Electrotherapy can provide temporary pain relief and help kickstart muscle activation, while ultrasound may assist in healing stubborn injuries. Importantly, these techniques are typically combined with active approaches like exercise and education to maximise results. While they may seem high-tech, both are safe, non-invasive, and painless treatments.
Dry Needling
Dry needling is a modern physiotherapy technique that uses very fine, sterile needles inserted into specific muscle points known as trigger points, targeting different muscles that may be contributing to pain . These are tight, irritable spots within a muscle that often cause referred pain or limit movement.
When a needle is inserted into a trigger point, it can create a local twitch response that helps release the tight band of muscle. This process reduces pain, improves blood flow, and restores normal muscle function. For patients, this often feels like a brief sharp sensation followed by a sense of relief or reduced tension in the area.
Dry needling can be particularly effective for conditions like pelvic pain, chronic neck and shoulder tension, headaches caused by muscle tightness, sports injuries, or lower back pain. It is usually performed as part of a broader physiotherapy plan, often alongside manual therapy and exercise. While some patients may feel slight soreness after treatment, this typically resolves within 24–48 hours and is a sign the muscle is resetting. Overall, dry needling is a safe and effective tool for targeting persistent muscular pain and dysfunction.
Education & Self-Management
Perhaps one of the most underrated but powerful aspects of physiotherapy, according to any health professional, is education. A key part of every physiotherapy session is helping you understand what’s happening in your body, why you’re experiencing pain, and providing personalised advice on how you can manage it. This knowledge empowers you to take an active role in your recovery, rather than relying solely on in-clinic treatment.
Your physiotherapist may educate you on topics such as posture, movement patterns, ergonomics at work, or lifestyle modifications that support healing. For example, office workers often benefit from advice on desk setup and strategies for breaking up long sitting periods, while athletes may learn about proper warm-up and recovery techniques to avoid re-injury.
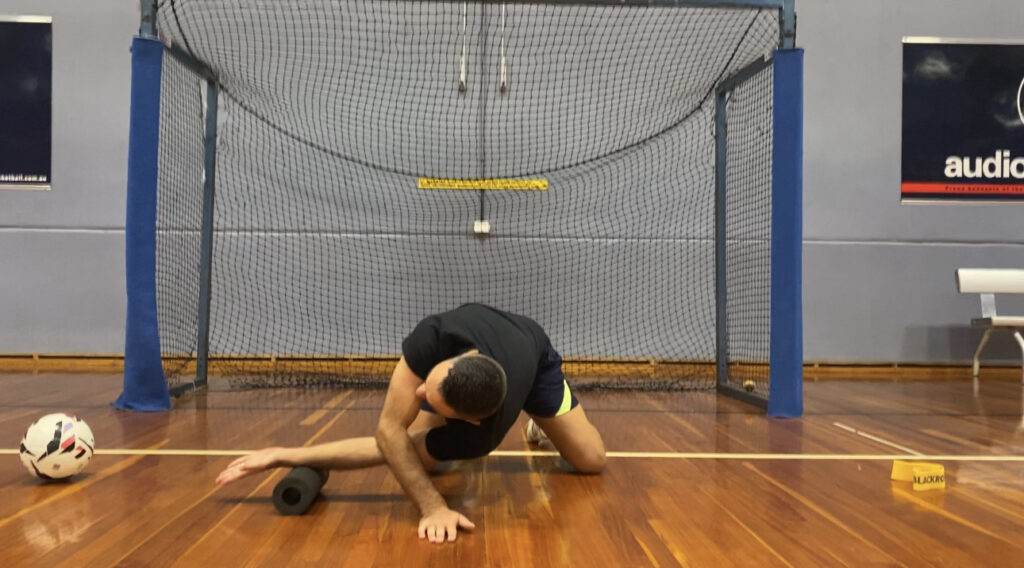
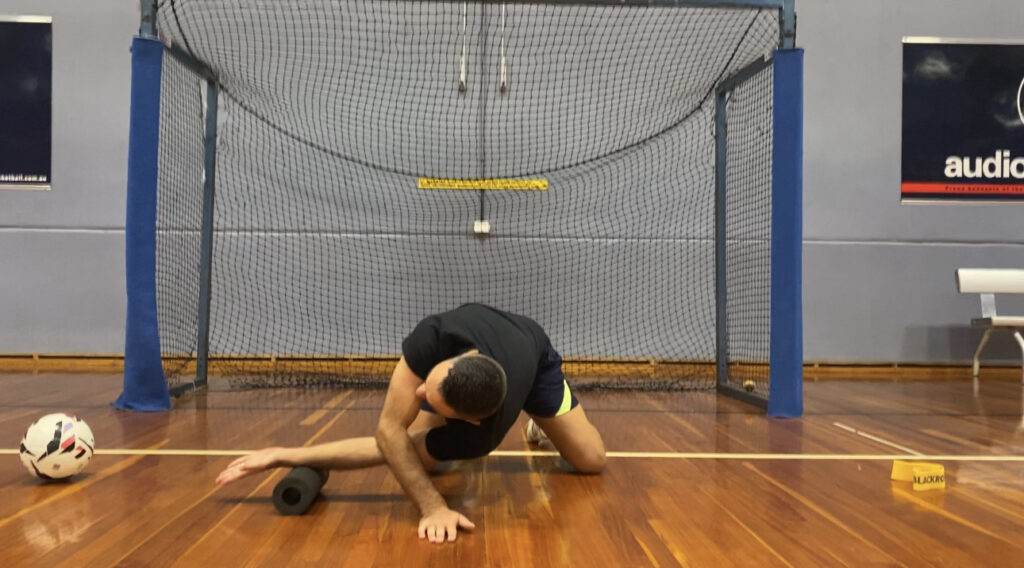
Self-management strategies might include a personalised home exercise plan, pacing daily activities, or using tools like foam rollers or heat packs between sessions. By following this advice consistently, you’re more likely to achieve long-term improvements and reduce the risk of recurring problems.
Education also helps reduce fear and uncertainty. When patients understand their condition, they often feel more in control and less anxious about recovery. In many cases, this shift in mindset is just as important as the physical treatment itself.
Addressing Common Concerns About Physiotherapy Sessions
Do I Need a Referral?
In most cases, no referral is needed. You can book directly with a physiotherapist.
What Should I Wear?
Wear comfortable clothing that allows easy movement, such as activewear or loose clothing.
How Many Sessions Will I Need?
This depends on your condition, but most people start noticing improvements within a few sessions.
Will It Hurt?
Some techniques may cause mild discomfort, especially if working on tight or injured areas, but physiotherapy should not be painful.
Cost and Private Health Cover
Physiotherapy is often covered by private health insurance. Check your fund for rebate details.
Preparing for Your First Physiotherapy Session
Bring Relevant Information
- Any scans, X-rays, or medical reports.
- A list of medications if relevant.
Dress Comfortably
- Choose clothing that gives your physiotherapist easy access to the problem area.
Prepare Questions to Ask
Examples include:
- What’s causing my pain?
- How long will recovery take?
- What can I do at home to help?
Conclusion: Take the First Step Towards Better Health
Your initial physiotherapy appointment is designed to make you feel informed, comfortable, and supported.
From the thorough assessment to the hands-on treatment and personalised plan, every step is focused on helping you achieve your goals.
Don’t let uncertainty hold you back. At Incline Health Leichhardt, our experienced team is here to guide you through the process with care and expertise.
Book your physiotherapy consultation today and know what to expect from your first appointment as you start your recovery journey with confidence.
FAQs
What happens during a physiotherapy session?
A session usually includes a quick review, hands-on treatment or exercise therapy, and advice on managing your condition at home.
How long do physio appointments normally take?
Initial appointments last about 45–60 minutes, and follow-ups are typically 30 minutes.
Book your physiotherapy consultation today and start your recovery journey with confidence.






